- Our Story
- Publications & Resources
- Publications & Resources
- Publications
- IEEE Signal Processing Magazine
- IEEE Journal of Selected Topics in Signal Processing
- IEEE Signal Processing Letters
- IEEE Transactions on Computational Imaging
- IEEE Transactions on Image Processing
- IEEE Transactions on Information Forensics and Security
- IEEE Transactions on Multimedia
- IEEE Transactions on Signal and Information Processing over Networks
- IEEE Transactions on Signal Processing
- IEEE TCI
- IEEE TSIPN
- Data & Challenges
- Submit Manuscript
- Guidelines
- Information for Authors
- Special Issue Deadlines
- Overview Articles
- Top Accessed Articles
- SPS Newsletter
- SigPort
- SPS Resource Center
- Publications FAQ
- Blog
- News
- Dataset Papers
- Conferences & Events
- Community & Involvement
- Professional Development
- For Volunteers
- Information for Authors-OJSP
-
Home
Conferences Events IEEE Signal Processing Magazine IEEE SPL Article IEEE TIFS Article IEEE TMM Article IEEE TSP Article Jobs in Signal Processing Lectures Machine Learning Seasonal Schools Signal Processing News SPM Article SPS Distinguished Lectures SPS Newsletter Article SPS Webinar SPS Webinars SPS Webinar Series Webinar webinars
-
Our Story
What is Signal Processing?
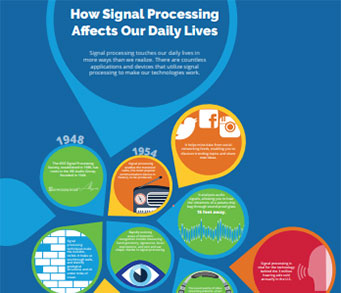
The technology we use, and even rely on, in our everyday lives –computers, radios, video, cell phones – is enabled by signal processing. Learn More » -
Publications & Resources
-
SPS Resources
- Signal Processing Magazine The premier publication of the society.
- SPS Newsletter Monthly updates in Signal Processing
- SPS Resource Center Online library of tutorials, lectures, and presentations.
- SigPort Online repository for reports, papers, and more.
- SPS Feed The latest news, events, and more from the world of Signal Processing.
-
SPS Resources
-
Conferences & Events
-
Community & Involvement
-
Membership
- Join SPS The IEEE Signal Processing Magazine, Conference, Discounts, Awards, Collaborations, and more!
- Chapter Locator Find your local chapter and connect with fellow industry professionals, academics and students
- Women in Signal Processing Networking and engagement opportunities for women across signal processing disciplines
- Students Scholarships, conference discounts, travel grants, SP Cup, VIP Cup, 5-MICC
- Young Professionals Career development opportunities, networking
- Get Involved
-
Technical Committees
- Applied Signal Processing Systems
- Audio and Acoustic Signal Processing
- Bio Imaging and Signal Processing
- Computational Imaging
- Image Video and Multidimensional Signal Processing
- Information Forensics and Security
- Machine Learning for Signal Processing
- Multimedia Signal Processing
- Sensor Array and Multichannel
- Signal Processing for Communication and Networking
- Signal Processing Theory and Methods
- Speech and Language Processing
- Technical Working Groups
- More TC Resources
-
Membership
-
Professional Development
-
Professional Development
- Signal Processing Mentorship Academy (SigMA) Program
- Micro Mentoring Experience Program (MiME)
- Distinguished Lecturer Program
- Distinguished Lecturers
- Distinguished Lecturer Nominations
- Past Lecturers
- Distinguished Industry Speaker Program
- Distinguished Industry Speakers
- Distinguished Industry Speaker Nominations
- Industry Resources
- IEEE Training Materials
- Jobs in Signal Processing: IEEE Job Site
-
Career Resources
- SPS Education Program Educational content in signal processing and related fields.
- Distinguished Lecturer Program Chapters have access to educators and authors in the fields of Signal Processing
- Job Opportunities Signal Processing and Technical Committee specific job opportunities
- Job Submission Form Employers may submit opportunities in the area of Signal Processing.
-
Professional Development
-
For Volunteers
-
For Board & Committee Members
- Board Agenda/Minutes* Agendas, minutes and supporting documentation for Board and Committee Members
- SPS Directory* Directory of volunteers, society and division directory for Board and Committee Members.
- Membership Development Reports* Insight into the Society’s month-over-month and year-over-year growths and declines for Board and Committee Members
-
For Board & Committee Members
Popular Pages
Today's:
- Information for Authors
- ICASSP@50: A Recap [Conference Highlights]
- (ICME 2026) 2026 IEEE International Conference on Multimedia and Expo
- IEEE Transactions on Information Forensics and Security
- IEEE Transactions on Multimedia
- IEEE Transactions on Image Processing
- Conference Call for Papers
- Information for Authors-SPL
- (ASRU 2025) 2025 IEEE Automatic Speech Recognition and Understanding Workshop
- IEEE Signal Processing Letters
- Building Bridges for Our Professional Future [President’s Message]
- Signal Processing Cup
- Submit a Manuscript
- IEEE JSTSP Special Issue on Advanced AI and Signal Processing for Low-Altitude Wireless Networks
- IEEE Transactions on Audio, Speech and Language Processing
All time:
- Information for Authors
- Submit a Manuscript
- IEEE Transactions on Image Processing
- IEEE Transactions on Information Forensics and Security
- IEEE Transactions on Multimedia
- IEEE Transactions on Audio, Speech and Language Processing
- IEEE Signal Processing Letters
- IEEE Transactions on Signal Processing
- Conferences & Events
- IEEE Journal of Selected Topics in Signal Processing
- Information for Authors-SPL
- Conference Call for Papers
- Signal Processing 101
- IEEE Signal Processing Magazine
- Guidelines
Last viewed:
- Submit Your 2026 ICASSP Workshop Paper
- ICASSP 2026 Call for Satellite Workshops
- IEEE Transactions on Signal Processing
- IEEE ISBI 2024 - Women in Signal Processing Event
- (CAI 2026) IEEE Conference on Artificial Intelligence 2026
- IEEE Transactions on Image Processing
- IEEE Transactions on Information Forensics and Security
- (ICME 2026) 2026 IEEE International Conference on Multimedia and Expo
- Conference Call for Papers
- Call for Proposals: IEEE ICME 2026
- Information for Authors
- Conferences & Events
- (ASRU 2025) 2025 IEEE Automatic Speech Recognition and Understanding Workshop
- New SPS Chapters in 2022
- Chapters
Modeling Obstructive Sleep Apnea Voices Using Deep Neural Network Embeddings and Domain-Adversarial Training
You are here
Journal of Selected Topics in Signal Processing
Publications & Resources
For Authors
Top Reasons to Join SPS Today!
1. IEEE Signal Processing Magazine
2. Signal Processing Digital Library*
3. Inside Signal Processing Newsletter
4. SPS Resource Center
5. Career advancement & recognition
6. Discounts on conferences and publications
7. Professional networking
8. Communities for students, young professionals, and women
9. Volunteer opportunities
10. Coming soon! PDH/CEU credits
Click here to learn more.
Modeling Obstructive Sleep Apnea Voices Using Deep Neural Network Embeddings and Domain-Adversarial Training
Obstructive Sleep Apnea (OSA) is a sleep breathing disorder affecting at least 3–7% of male adults and 2–5% of female adults between 30 and 70 years. It causes recurrent partial or total obstruction episodes at the level of the pharynx which causes cessation of breath during sleep. The number of obstruction episodes per sleep hour, known as Apnea-Hypopnea Index (AHI), along with the degree of the daytime sleepiness, determine the severity of OSA. Usually, OSA is diagnosed at a Sleep Unit in a hospital by the time-consuming polysomnography (PSG) test. Based on the expected impact of anatomical and physiological effects of the altered structure of the upper airway in OSA patients’ voices, the assessment of OSA from speech has been proposed as a simple way to help in the diagnostic process. In this paper, we review previous research to assess OSA from speech and underline the difficulty of a weak connection between OSA and speech. We present results to model OSA using, to the best of our knowledge, for the first time Deep Learning on the largest existing database of OSA voice recordings and speakers’ clinical variables. Using state-of-the-art speaker recognition techniques: acoustic subspace modeling (i-vectors), and deep neural network embeddings (x-vectors), we confirm the weak connection between speech and OSA. We hypothesize that this weak effect is mediated by undesired sources of variability as speakers’ age, body mass index (BMI), or height, and we propose Domain-Adversarial Training (DAT) to remove them. Our results show that, taking BMI as adversarial domain, when classifying voices from OSA extreme cases (AHI $\leq$ 10 vs. AHI $\geq$ 30) accuracy increases from 69.39% to 76.60%. We hope these results can encourage the use of adversarial-domain neural networks to remove the undesired effects of clinical variables or other speaker factors when assessing health disorders from speech.
SPS Social Media
- IEEE SPS Facebook Page https://www.facebook.com/ieeeSPS
- IEEE SPS X Page https://x.com/IEEEsps
- IEEE SPS Instagram Page https://www.instagram.com/ieeesps/?hl=en
- IEEE SPS LinkedIn Page https://www.linkedin.com/company/ieeesps/
- IEEE SPS YouTube Channel https://www.youtube.com/ieeeSPS
Home | Sitemap | Contact | Accessibility | Nondiscrimination Policy | IEEE Ethics Reporting | IEEE Privacy Policy | Terms | Feedback
© Copyright 2025 IEEE - All rights reserved. Use of this website signifies your agreement to the IEEE Terms and Conditions.
A public charity, IEEE is the world's largest technical professional organization dedicated to advancing technology for the benefit of humanity.











